What is Activity PRN?
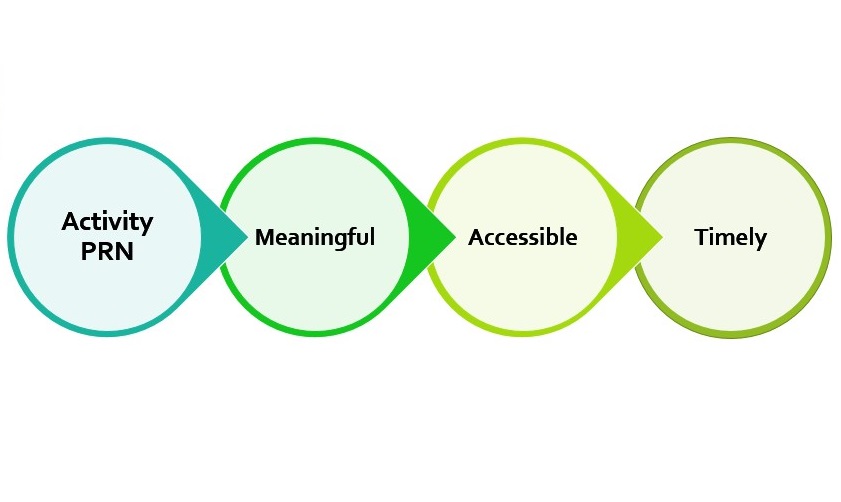
It’s a process of using Occupational Therapy practices to facilitate engagement in meaningful and accessible activities, as and when required [*Derived from the Latin phrase “pro re nata,” PRN stands for “when necessary”]. I felt that individuals could benefit from engaging in planned activities as a distraction technique or as a coping strategy.
Why are activities important in daily life?
We all have daily activities that we want and need to do on a daily basis. Humans are occupational beings, and often define themselves by what they do. Different activities allow us to express ourselves in a practical way. By engaging in activities that you enjoy, are good at, or by learning new activities, you can feel a sense of accomplishment, which positively impacts on your mental health.
Where did the idea come from? What inspired it?
The inspiration came from PRN medication which is available as and when required to support individuals on the PICU when experiencing a crisis. When I first started to work on mental health wards, I noticed that due to a more restrictive environment, for safety reasons, materials to engage in activities were not always freely and easily available.
I came up with the idea of ‘prescribing’ activities to individuals, and to prep and ready those activities for when they were needed. Individuals would receive a PRN card that lists the activities, as well as what materials are needed and where they are stored. That way, healthcare staff would have the information needed to support them during times when they might not be engaging in meaningful activities or in therapy groups.
Who are the key players?
I developed a protocol and implemented it on Bearsted Ward, but the other key players are our ward staff who support individuals on a daily basis. Individuals need to be engaged in meaningful activity, and the staff hold the materials and the skills to support them, creating a wonderful working partnership on the ward. Hospital management were very supportive by backing the project and supply of activity resources.
How can individuals maintain the practice after discharge?
I would recommend they have a list of activities that they enjoy doing, and some materials prepped and accessible for when they need them. This could be an ‘activity box’ at home, a mindful colouring book and pens on the coffee table, a baking box ready to be made up and put in the oven, or a playlist of music saved on their phone. They can use a visual prompt such as a card or poster to remind them.
How can carers get involved to support their loved one?
Families, carers and friends provide vital information and support, as they know their loved ones the most. It might be helpful to suggest activities that the individual previously enjoyed doing, or provide insight into how they are best supported to engage in activities. This approach can also be used after discharge, by arranging the required support and resources so that the individual can continue to engage in activities as and when required.
Neil’s published article can be read in full here.